Provider Enrollment
Mission
Increase Georgia’s Medicaid provider enrollment and retention by reducing barriers to an expedient and consistent user experience.
- Meeting Schedule: The Provider Enrollment Workgroup meets on the second Wednesday of every month.
- Meeting Time: 11:15 a.m. to 12:15 p.m.
- Agenda Requests: To ensure that our discussions align with the needs of all stakeholders, we request agenda items at the end of each meeting.
Electronic Provider Notification
- Existing problem: Welcome letters are mailed to providers when they are approved and added to the CMO contracts. The physical letter is often lost in transit, and the providers are unaware that they can begin providing services to Medicaid patients.
- Identified solution: AG and PSHP will begin emailing providers welcome letters in Spring 2024. CS is meeting internally to determine if this is a project they can undertake.
Therapy Provider Notifications
- Existing problem: When new providers are added to existing therapy contracts, enrollment notification letters are not being sent.
- Identified solution: AG and PSHP have identified the system flaw that prevented these welcome letters from being sent out. System updates have taken place, and letters are currently being tracked for providers enrolled in the Trialliance Therapy Group beginning December 2023.
Delegated Roster
- Final updates to the Delegated Roster survey are underway. The new survey will be sent to Delegated Roster Entities in February 2024.
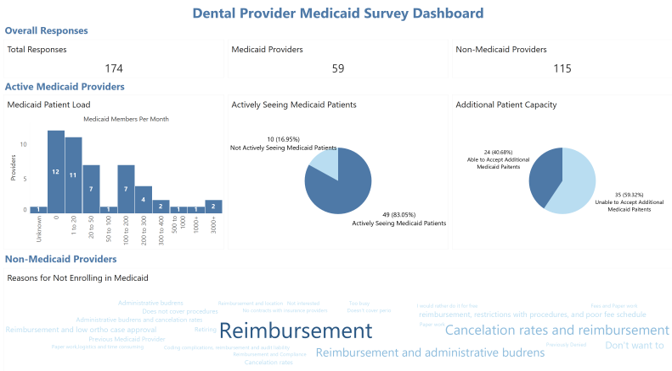
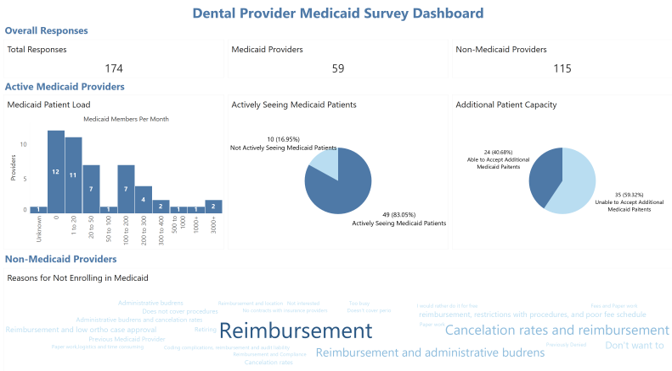
In our Provider Enrollment workgroup, we created a survey to understand the number of dental providers who are not enrolled in Medicaid and better understand the reasons for not doing so. To no surprise, it is overwhelmingly due to reimbursement fees, but also cancelation rates and admin burdens. We also heard many concerns about ‘ghost providers,’ those enrolled in Medicaid but not seeing Medicaid patients. This survey attempted to capture that trend as well.
We are looking to get a greater response rate, but in the meantime, we are working with DMOs to determine ways to incentivize enrollment in Medicaid and to continue seeing patients.