
What is Lupus
What is Lupus?

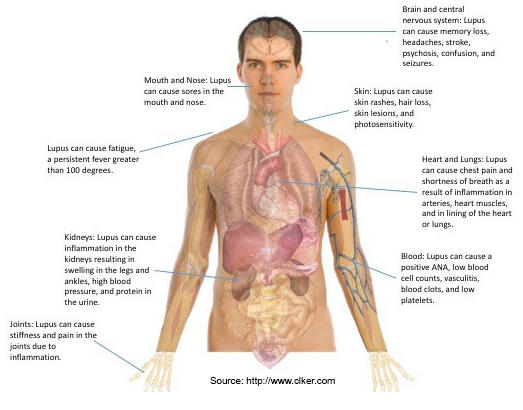
Lupus Erythematosus is a chronic autoimmune disease that causes the immune system to attack one’s body. The disease is characterized by the inflammation of various healthy tissues and organs in the body, including the joints, skin, kidneys, heart, lungs, blood vessels and brain. The severity of the disease may vary because no two cases of lupus are exactly alike.
What are the different types of Lupus?
Systemic Lupus Erythematosus (SLE) is the type of the disease that can affect many parts of the body. SLE is the most common form of the disease and is most commonly characterized by inflammation to the joints, skin, kidneys, heart, lungs, blood vessels and brain.
Cutaneous Lupus Erythematosus is a chronic skin disorder than can affect the skin. Patients with Cutaneous Lupus develop photosensitivity, hair loss, skin rashes and skin lesions.
Drug-Induced Lupus Erythematosus, like SLE, can affect many parts of the body. However, Drug-Induced Lupus is caused by an overreaction to certain medications. Studies have shown that removal of the medication may stop disease activity. Drugs most commonly connected with drug-induced lupus are those used to treat chronic conditions, such as seizures, high blood pressure or rheumatoid arthritis.
Neonatal Lupus Erythematosus occurs when auto-antibodies from a mother living with SLE passively transfer to the infant. Like SLE, Neonatal Lupus can affect many parts of the body including the skin, liver and blood. These symptoms disappear completely after several months and have no lasting effects.
What causes Lupus?
The causes of lupus are unknown, but are believed to be linked to genetic, environmental and hormonal factors. In some families, inherited factors play a role in a person’s risk for developing lupus.
Who gets Lupus?
Anyone can have lupus. More than 90 percent of people living with lupus are women between the ages of 15 and 45. African-American, Hispanic, Asian and Native American women are at greater risk of developing lupus than white women. In particular, African-American women are three times more likely to get lupus than white women. Men, who make up 10 percent of lupus patients, often develop the disease before puberty and after the age of 50.
Is Lupus contagious?
Lupus is not contagious or infectious, and therefore cannot be transmitted to other people.
What is a Lupus flare?
Most patients have times when the disease is active or in a flare, followed by times when the disease is less active or in a remission. Understanding how to prevent flares and how to treat them when they do occur helps people with lupus maintain better health.
Is there a cure for Lupus?
There is no cure for lupus. However, there are treatments that can help prevent flares, treat symptoms and reduce organ damage.
Is Lupus fatal?
Many men and women live long, productive lives with lupus. It is fatal in some people. It depends on the severity of the disease, how the body responds to treatments, and other factors. Infections, cardiovascular disease and kidney failure are common complications and the most common causes of death in people with lupus.
Systemic Lupus Erythematosus (SLE)
What are the common symptoms of SLE?
How is SLE diagnosed?
SLE is chronic and complex, and is often difficult to diagnose. First, there is no single laboratory test that can determine if a person has SLE. Second, many symptoms of SLE are similar to those of other diseases, and can come and go over weeks and months. Finally, doctors must look at a person’s medical history, rule out other diseases, and consider both physical and laboratory evidence before a SLE diagnosis. The symptoms of SLE vary from patient to patient.
Eleven Criteria of Lupus
The American College of Rheumatology established “Eleven Criteria of Lupus” to help make or exclude a diagnosis of SLE. If your doctor finds that you have at least four of the eleven symptoms listed below and finds no other reason for them, you may have SLE.
- Malar rash: butterfly-shaped rash across cheeks and nose
- Discoid (skin) rash: raised red patches
- Photosensitivity: skin rash as result of unusual reaction to sunlight
- Mouth or nose ulcers: usually painless
- Arthritis (nonerosive) in two or more joints, along with tenderness, swelling or effusion. With nonerosive arthritis, the bones around joints don’t get destroyed.
- Cardio-pulmonary involvement: inflammation of the lining around the heart (pericarditis) and/or lungs (pleuritis)
- Neurologic disorder: seizures and/or psychosis
- Renal (kidney) disorder: excessive protein in the urine or cellular casts in the urine
- Hematologic (blood) disorder: hemolytic anemia, low white blood cell count or low platelet count.
- Immunologic disorder: antibodies to double stranded DNA, antibodies to Sm, or antibodies to cardiolipin
- Antinuclear antibodies (ANA): a positive test in the absence of drugs known to induce it.
Cutaneous Lupus Erythematosus (CLE)
What are the common symptoms of CLE?
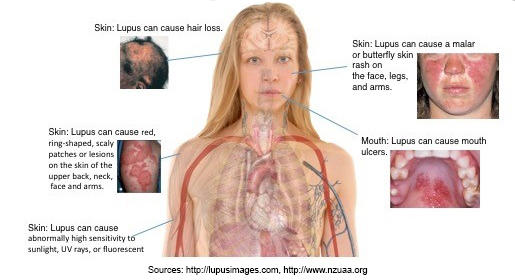
Cutaneous Lupus Erythematosus (Cutaneous Lupus) causes photosensitivity, skin rashes and skin lesions on any part of the body. There are three common types of Cutaneous Lupus, Discoid Lupus, Subacute Cutaneous Lupus and Acute Cutaneous Lupus.
Discoid Lupus:
Discoid Lupus is the most common form of Cutaneous Lupus. People living with Discoid Lupus complain of a red, raised and scaly lesion on the face, scalp or parts of the body. Manifestations on the face form across the cheeks, nose and ears. Over time, these lesions can produce scarring and skin discoloration (darkly colored and/or lightly colored areas). Typically, these lesions occur on areas of the body that are exposed to sunlight or fluorescent lights. If lesions appear in the scalp or involve the hair follicles, areas of hair loss may develop which could be permanent if the hair follicle is completely destroyed. They are often not itchy or painful.
Subacute Cutaneous Lupus:
Subacute Cutaneous Lupus can cause skin lesions on any part of the body. These lesions often form red, ring-shaped, scaly patches on the skin. These lesions do not itch and often appear on the chest as well as the upper back and neck; however, they may also be seen on the face and arms. Typically, these lesions occur on areas of the body that are exposed to sunlight or fluorescent lights. Furthermore, it is not uncommon for patients with SCLE to have associated joint disease.
Acute Cutaneous Lupus:

Acute Cutaneous Lupus results in flat red patches on the cheeks and nose called a malar or butterfly rash that looks quite like sunburn. These patches may also appear on the arms, legs, trunk and any other area that is commonly exposed to the sun. Patients with Acute Cutaneous Lupus can also manifest oral ulcers, hives and temporary hair loss. Acute Cutaneous Lupus is more common in people living with SLE.
How is Cutaneous Lupus diagnosed?
A skin biopsy is helpful in making the diagnosis of Cutaneous Lupus in addition to direct immunofluorescence tests, which reveal antibody deposition within the skin.
Who gets Cutaneous Lupus?
Cutaneous lupus most often affects women ages 20-50. Two-thirds of people living with SLE will develop some type of Cutaneous Lupus. Manifestations of skin disease are often induced by sunlight.
Treatment
While there is no cure for lupus, there are treatments that can help prevent flares, treat symptoms and reduce organ damage. Early diagnosis and treatment is the key to successful management of lupus. Treatment depends on the type and severity of the symptoms. Like all medications, these treatments have potential side effects. It is very important that you communicate with your health care professional about the potential benefits and potential side effects of any treatment.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs):
NSAIDs, like ibuprofen (Aleve, Motrin, Advil), decrease swelling, pain and fever. Always check with your doctor before taking any medications that are over the counter (without a prescription) for your lupus.
-
Antimalarial drugs:
Antimalarials, such as hydroxychloroquine (Plaquenil), help relieve some lupus symptoms, such as fatigue, rashes, joint pain or mouth sores. Research has shown that antimalarials can prevent abnormal blood clotting, modify the course of the disease, prevent progression and slow joint damage.
-
Corticosteroids:
Corticosteroids, such as prednisone, suppress the immune system and are often used in patients with serious or life-threatening inflammation in major organs such as the kidneys, lungs, and heart. Patients with Cutaneous Lupus may also be treated with corticosteroid injections, creams or ointments.
-
Immune Suppressants:
Immune suppressants, such as azathioprine (Imuran), cyclophosphamide (Cytoxan), methotrexate (Trexall), mycophenolate (CellCept) and cyclosporine (Neoral), suppress the immune system and are often used in patients with serious or life-threatening inflammation in major organs such as the kidneys, lungs and heart.
- Biologics:
Biologics, such as Benlysta, block a protein that prolongs the survival of autoantibody-producing B cells, which are the antibodies that target the body’s own tissues. Unlike immune suppressants and corticosteroids, biologics target specific cells in the immune system.
-
Sunscreen:
Many people living with lupus are photosensitive or sensitive to the sun and fluorescent lights. It is recommended that all people living with lupus wear sunscreen. Sunscreens, greater than SPF 30, are vital in protecting patients from UVA and UVB rays which provoke skin rashes, lesions and other lupus disease activity. Patients should also avoid excess sun exposure by wearing sunscreen, wide-brim hats, avoid sunlight during peak hours of UV exposure (10:00 am - 2:00 pm) and wear tightly woven clothing.
-
Diet, Rest and Exercise:
Persons living with lupus should include a diet made up of fruits, vegetables and whole grains, as well as low-fat dairy and lean sources of protein, as a part of their daily routine. A medically supervised exercise program, balanced with rest, is also essential to the treatment plan.