
Network Adequacy
Geographic Access Standards and Reports
The Department of Community Health currently contracts with the following three Care Management Organizations (CMOs) to deliver services to Medicaid members: Amerigroup, CareSource, and Peach State Health Plan. All 3 CMOs serve members residing in communities throughout the state of Georgia.

Each CMO is required to develop and maintain a network of Providers and Facilities adequate to deliver Covered Services while ensuring adequate and appropriate provision of services to members under the Georgia Families Contract. To demonstrate that the requirement has been met, CMOs must conduct a geographic access analysis of their network utilizing the standards as outlined in Figure 1 of the Georgia Families Contract below:
| Provider Type | Urban | Rural |
|---|---|---|
| PCPs* | Two (2) within eight (8) miles | Two (2) within fifteen (15) miles |
| Pediatricians | Two (2) within eight (8) miles | Two (2) within fifteen (15) miles |
| Obstetric Providers | Two (2) within thirty (30) minutes or thirty (30) miles | Two (2) within forty-five (45) minutes or forty-five (45) miles |
| Specialists | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
| General Dental Providers | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
| Dental Subspecialty Providers | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
| Hospitals | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
| Mental Health Providers | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
| Pharmacies | One (1) twenty-four (24) hours a day, seven (7) days a week within fifteen (15) minutes or fifteen (15) miles | One (1) twenty-four (24) hours a day (or has an afterhours emergency phone number and pharmacist on call), seven (7) days a week within thirty (30) minutes or thirty (30) miles |
| Therapy: Physical Therapists, Occupational Therapists and Speech Therapists | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
| Vision Providers | One (1) within thirty (30) minutes or thirty (30) miles | One (1) within forty-five (45) minutes or forty-five (45) miles |
*PCPs not including practitioners listed below in Table.
The CMOs submit Network Adequacy Reports which provide member access data by county on a quarterly basis. Georgia requires that at least 90% of the members in each county have access to a provider when the contractual access standards are applied. In counties where access is below 90%, CMOs are required to provide a corrective action plan to address the deficiency. Corrective actions include recruiting additional providers where providers are available, contracting with providers in nearby counties to fills the gaps in access, or coordinating non-emergency transportation services, as necessary, to ensure that members receive care.
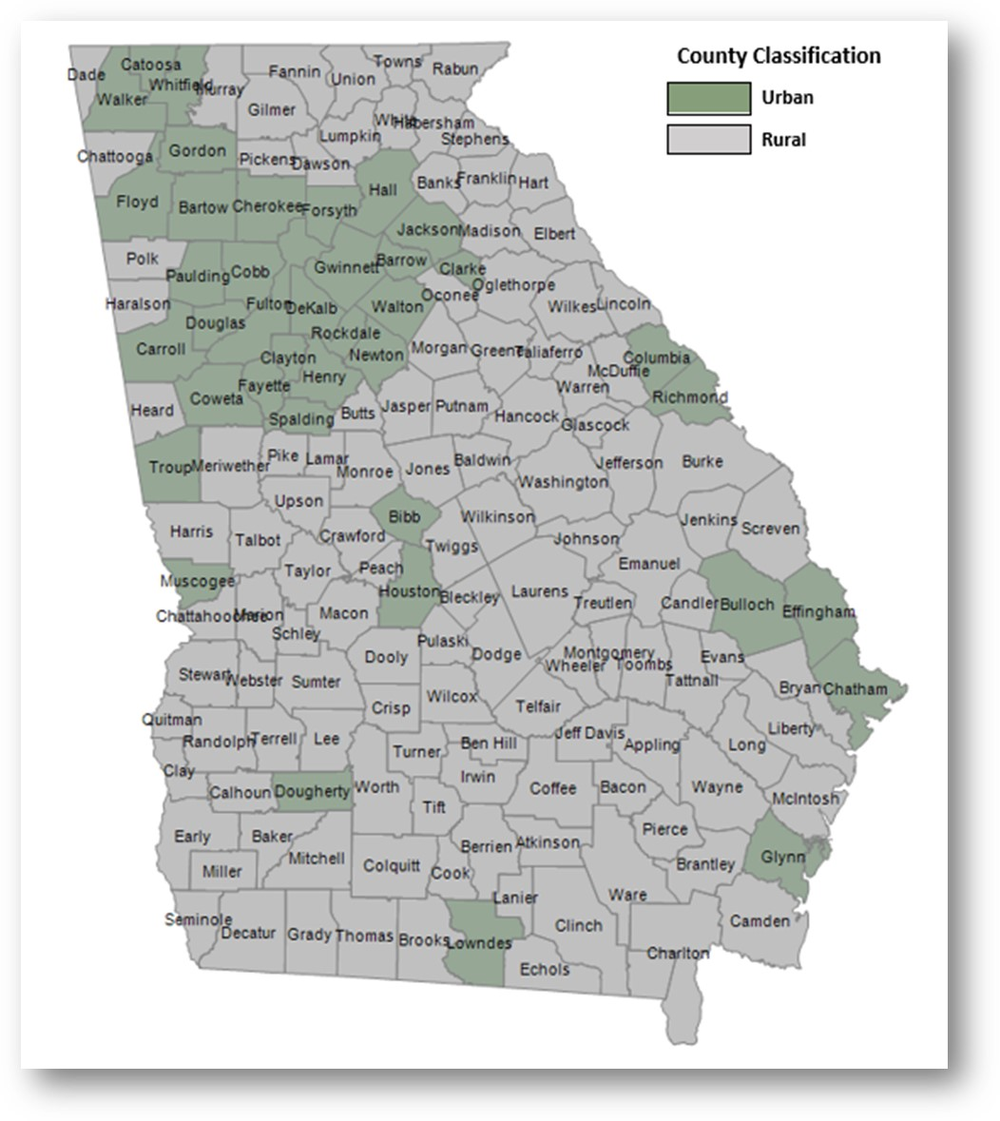
The reports are broken down by managed care region. Georgia has six (6) managed care regions: Atlanta, Central, East, North, Southeast, and Southwest. The counties contained within each region are classified as urban or rural as shown in the Georgia county map below.
Network Adequacy Reports
Network Adequacy Reports from prior years can be accessed here.
Amerigroup
-
6004_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q4_20250129
-
6004_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q4_20250129
-
6004_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q4_20250129
-
6004_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q4_20250129
-
6004_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q4_20250129
-
6004_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q4_20250129
-
6004_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q3_20241030
-
6004_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q3_20241030
-
6004_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q3_20241030
-
6004_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q3_20241030
-
6004_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q3_20241030
-
6004_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q3_20241030
-
6004_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q2_20240809.
-
6004_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q2_20240809
-
6004_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q2_20240809
-
6004_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q2_20240809
-
6004_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q2_20240809
-
6004_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q2_20240809
-
6004_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q1_20240515
-
6004_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q1_20240515
-
6004_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q1_20240515
-
6004_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q1_20240515.
-
6004_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q1_20240515.
-
6004_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q1_20240515
CareSource
-
6005_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q4_20250130
-
6005_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q4_20250130
-
6005_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q4_20250130
-
6005_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q4_20250130
-
6005_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q4_20250130
-
6005_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q4_20250130
-
6005_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q3_20241030
-
6005_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q3_20241030
-
6005_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q3_20241030
-
6005_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q3_20241030
-
6005_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q3_20241030
-
6005_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q3_20241030
-
6005_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q2_20240911
-
6005_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q2_20240911
-
6005_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q2_20240911
-
6005_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q2_20240911
-
6005_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q2_20240911
-
6005_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q2_20240911
-
6005_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q1_20240429
-
6005_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q1_20240429
-
6005_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q1_20240429
-
6005_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q1_20240429
-
6005_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q1_20240429
-
6005_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q1_20240429
Georgia Families 360
-
6008_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q4_20250129
-
6008_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q4_20250129
-
6008_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q4_20250129
-
6008_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q4_20250129
-
6008_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q4_20250129
-
6008_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q4_20250129
-
6008_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q3_20241206
-
6008_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q3_20241030
-
6008_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q3_20241030
-
6008_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q3_20241030
-
6008_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q3_20241030
-
6008_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q3_20241030
-
6008_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q2_20240809
-
6008_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q2_20240809
-
6008_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q2_20240809
-
6008_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q2_20240809
-
6008_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q2_20240809
-
6008_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q2_20240809
-
6008_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q1_20240515
-
6008_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q1_20240515
-
6008_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q1_20240515
-
6008_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q1_20240515
-
6008_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q1_20240515
-
6008_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q1_20240515
Peach State Health Plan
-
6006_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q4_20250130
-
6006_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q4_20250130
-
6006_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q4_20250130
-
6006_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q4_20250130
-
6006_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q4_20250130
-
6006_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q4_20250130
-
6006_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q3_20241030
-
6006_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q3_20241030
-
6006_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q3_20241030
-
6006_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q3_20241030
-
6006_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q3_20241030
-
6006_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q3_20241030
-
6006_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q2_20240730
-
6006_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q2_20240730
-
6006_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q2_20240730
-
6006_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q2_20240730
-
6006_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q2_20240730
-
6006_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q2_20241003
-
6006_CCR-013O_GeoAccess County Detail Report AT_Quarterly_2024Q1_20240430
-
6006_CCR-013P_GeoAccess County Detail Report CN_Quarterly_2024Q1_20240430
-
6006_CCR-013Q_GeoAccess County Detail Report E_Quarterly_2024Q1_20240430
-
6006_CCR-013R_GeoAccess County Detail Report N_Quarterly_2024Q1_20240430
-
6006_CCR-013S_GeoAccess County Detail Report SE_Quarterly_2024Q1_20240430
-
6006_CCR-013T_GeoAccess County Detail Report SW_Quarterly_2024Q1_20240430
Georgia County Map
Network Accessibility Standards
Network accessibility standards establish the maximum amount of time a member should have to wait to obtain an appointment with a participating provider based on the type and urgency of the service requested.
The CMOs must have in its network the capacity to ensure that waiting times for appointments do not exceed those outlined in Figure 2 of the Georgia Families Contract below.
| Provider Type | Waiting Time |
|---|---|
| PCPs (routine visits) | Not to exceed fourteen (14) calendar days |
| PCP (adult sick visit) | Not to exceed twenty-four (24) clock hours |
| PCP (pediatric sick visit) | Not to exceed twenty-four (24) clock hours |
| Maternity Care | First Trimester – Not to exceed fourteen (14) calendar days Second Trimester – Not to exceed seven (7) calendar days Third Trimester – Not to exceed three (3) business days |
| Specialists | Not to exceed thirty (30) calendar days |
| Therapy: Physical Therapists, Occupational Therapists, Speech Therapists, Aquatic Therapists | Not to exceed thirty (30) calendar days |
| Vision Providers | Not to exceed thirty (30) calendar days |
| Dental Providers (routine visits) | Not to exceed twenty-one (21) calendar days |
| Dental Providers (Urgent Care) | Not to exceed forty-eight (48) clock hours |
| Elective Hospitalizations | Thirty (30) calendar days |
| Mental Health Providers | Fourteen (14) calendar days |
| Urgent Care Providers | Not to exceed twenty-four (24) clock hours |
| Emergency Providers | Immediately (twenty-four (24) clock hours a day, seven (7) days a week) and without prior authorization |